The study examined the association between baseline hemoglobin concentration and a range of cardiovascular clinical outcomes in a broad cohort of 39,922 patients across the spectrum of ACS. A total of 25,419 patients with STEMI and 14,503 patients with NSTE ACS whose baseline hemoglobin data was available were examined. These patients were divided into categories based upon increments of their hemoglobin levels.
In patients with STEMI, the likelihood of hypotension, tachycardia and Killip class II or IV was significantly related to baseline hemoglobin (P<0.001), with patients at either end of the hemoglobin spectrum having a higher likelihood of hemodynamic disarray. After adjustments for baseline characteristics, it was found a reverse J shaped relationship between baseline hemoglobin values and major adverse cardiovascular events. More specifically, in patients with ST-elevation myocardial infarction, cardiovascular mortality increased as hemoglobin levels fell below 14 g/dL (OR of 1.21 and 95% CI 1.12 to 1.30, P<0.001) for each 1-g/dL decrement in hemoglobin. Likewise for patients with hemoglobin values great than 17 g/dL there was also increased mortality (OR 1.79, 95% CI 1.18 to 2.71, P=0.007). In patients with NSTE ACS, the likelihood of cardiovascular death, myocardial infarction or recurrent ischemia increased as the hemoglobin fell below 11 g/dL, with an OP of 1.45 (95% CI 1.33 to 1.58, P>0.001) for each 1 g/dL decrement in hemoglobin. Patients with hemoglobin levels greater than 16 g/dL also had an increased rate of death or ischemic event (OR 1.31, 95% CI 1.03 to 1.66, P=0.027).
In this broad cohort of patients with ACS, the study found highly significant associations between low hemoglobin concentrations and adverse cardiovascular outcomes, such as prevalence of hypotension, tachycardia and Killip class II or IV. Among patients with STEMI, there was an increase in mortality and heart failure as the baseline hemoglobin dropped below 14 g/dL. In patients with NSTE ACS, and increased odds ratio of cardiovascular death, MI or recurrent ischemia became apparent when the baseline hemoglobin fell below 11 g/dL.
Anemia has been shown to significantly decrease oxygen delivery to the myocardium and increase the myocardial oxygen demand through necessitating a higher stroke volume and heart rate. The combination of these processes may explain the pathophyiology underlying the progressively worse outcomes observed in patients with ACS and lower baseline hemoglobin concentrations. In patients with very high hemoglobin levels (>17 g/dL), the increase in blood viscosity can lead to an increase in coronary vascular resistance and a decrease coronary blood flow, which can ultimately lead to thrombosis and MI.
There have been many previous studies that indicated a significant improvement of anginal symptoms with PCI in patients with coronary artery disease. However, this study focused on the improvement of mortality and risk of subsequent myocardial infarction in patients who underwent PCI compared to those who underwent medical therapy.
A total of 2950 patients were included in the meta-analysis (1476 received PCI, and 1474 received conservative treatment). There was no significant difference between the 2 treatment strategies with regard to mortality, cardiac death or myocardial infarction, nonfatal myocardial infarction, CABG, or PCI during follow-up. By random effects, the risk ratios (95% CIs) for the PCI versus conservative treatment arms were 0.94 (0.72 to 1.24), 1.17 (0.88 to 1.57), 1.28 (0.94 to 1.75), 1.03 (0.80 to 1.33), and 1.23 (0.80 to 1.90) for these 5 outcomes, respectively. A possible survival benefit was seen for PCI only in trials of patients who had a relatively recent myocardial infarction (risk ratio 0.40, 95% CI 0.17 to 0.95).
The study thus indicates there is no significant difference in mortality or risk of MI in patients who underwent PCI as compared to patients who underwent conservative medical treatment. When comparing such treatment options, one must consider the greater financial cost and risk of in-hospital mortality with PCI. While symptoms may improve, the patient's longevity does not increase with PCI.
Congestive heart failure and atrial fibrillation often coexist, each promoting the existence of the other. When trying to maintain sinus rhythm in patients with atrial fibrillation complicated by congestive heart failure, antiarrhythmic drugs often prove to have low efficacy or potentially harmful side effects. This study evaluated the effects of restoring and maintaining sinus rhythm via catheter ablation in this subgroup of patients in order to avoid the use of antiarrhythmic drugs.
In the study, investigators enrolled 58 consecutive patients with congestive heart failure of NYHA Class II who were undergoing curative ablation for atrial fibrillation that was resistant to at least two antiarrhythmic drugs and had a left ventricular ejection fraction of less than 45 percent. These patients were matched for age, sex, and classification of atrial fibrillation with procedural controls during the same time period from March 2001 to March 2004.
Patients were admitted two days prior to ablation and oral anticoagulants were stopped on admission. Anti-arrhythmic drugs were stopped prior to the procedure. Heart rate and rhythm were monitored by 48 hour ambulatory electrocardiography, and transesophageal echocardiography was performed to rule out atrial thrombi prior to ablation. Transthoracic echocardiography was used to assess left ventricle size and function. The ablation procedure aimed to electrically isolate all the pulmonary veins and to create a complete obstacle to electrical conduction. Post-ablation, anticoagulation therapy was reinitiated, and patients were monitored for three days. Patients were also tested for baseline exercise capacity on a bicycle stress test.
Follow-up required rehospitalization at 1, 3, 6, and 12 months after the last ablation procedure, and consisted of clinical interviews, 48-hour electrocardiographic monitoring, transthoracic echocardiography, and exercise testing. Anticoagulation was discontinued if sinus rhythm was maintained for three to six months. Symptoms and quality of life were assessed at 3 and 12 months.
The results of the study showed an improvement in cardiac function after establishing and maintaining sinus rhythm from catheter ablation. NYHA congestive heart failure class improved from a mean of 2.3 to 1.4 at the one month mark, and stayed at that level. Exercise time and capacity increased significantly, from mean time of 11 minutes to 15 minutes (P<0.001) and mean maximal capacity from 123 to 144 W (P<0.001) during the follow-up period. The left ventricular ejection fraction increased by a mean of 21 percent, with the greatest improvement seen in the first three months. The Symptom Checklist-Frequency and Severity scores and SF-36 quality of life measures improved significantly as well.
In conclusion, after catheter ablation for atrial fibrillation, long term restoration of sinus rhythm, without the use of antiarrhythmic drugs, resulted in significant improvement in left ventricular function, exercise capacity, symptoms, and quality of life. Furthermore, while this study did not directly assess the effect on mortality, because a reduced ejection fraction is an important predictor of mortality, the significant improvement in left ventricular function after ablation could be important in improving survival.
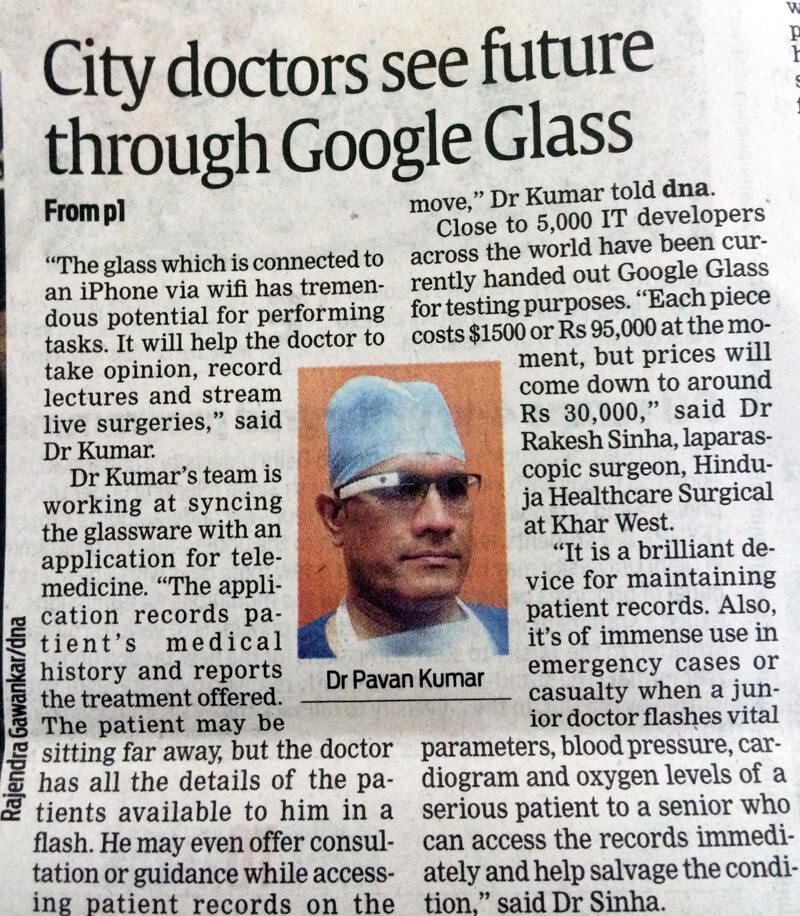
Dr. Pavan Kumar is performing a Surgery of Heart Valve Replacement on September 26, 2004. The day is being celebrated as the World Heart Day and as such the surgery will be live telecast.
Moderate and high levels of physical activity can reduce the risk of having a stroke, according to an analysis of studies on the topic.
The researchers pooled the results of 23 studies that examined physical activity in relation to stroke incidence or mortality.
As they report, the combined data showed that active or fit subjects had a reduced stroke risk compared with inactive or unfit subjects.
Depending on the type of study included in the analysis, individuals with high levels of activity had a 25 to 64 percent lower risk of stroke or death compared with subjects with low activity levels. Overall, when all the studies were combined, the risk reduction was 27 percent.
Furthermore, moderately and highly active individuals had lower risk of both of the main types of stroke (caused by artery blockage or by bleeding in the brain) than low- active individuals.
It is now established beyond reasonable doubt that high-level physical activity is to be strongly recommended for the prevention of stroke.
Individuals 75 years of age and older can have similar benefit from coronary artery bypass surgery as compared to younger patients.
A coronary artery bypass graft (CABG) is a surgical treatment for coronary artery disease (CAD), a chronic disease in which there is a hardening and narrowing (atherosclerosis) of the coronary arteries. During CABG, a surgeon takes a segment of a healthy blood vessel (either an artery or vein) from another part of the body, and uses it to create a detour or bypass around the blocked portion of the coronary artery. As a result, oxygen-rich blood can flow more freely to nourish the heart muscle. A patient may undergo one, two, three or more bypasses depending on how many coronary arteries (and their main branches) are blocked.
The CABG is the most commonly performed surgery in the United States and around the world. Bypass surgery may be recommended to individuals with a history of any of the following:
- Narrowing in several coronary artery branches (common in diabetics)
- Severe narrowing in the left main coronary artery
- Blockage or other condition that may not or has not responded to other treatments (e.g., angioplasty)
- Severe angina
Although there are risks associated with any surgery, the potential life-saving benefits of a CABG usually outweigh the risks.
Despite increasing use of CABG in the elderly, few data exist about elderly patients' health status benefits from CABG." The researchers analyzed health data and questionnaires for 690 patients enrolled in the study. Of these, 156 were over 75 years of age; 534 were 75 years or younger.
Results showed that both groups had "substantial improvement" in their health status at one year following CABG, although the elderly patients' had a slower rate of physical function. Both groups also had "rapid" and "sustained" relief from angina. In addition, both groups had significant improvement in overall quality of life.
The researchers conclude that "age alone does not appear to exert an important influence on the health status outcomes of CABG." The decision whether to do the procedure should consider, according to the researchers, the "potential for [CABG] to improve patients' symptoms, function, and quality of life" along with the known risks of the procedure and an expected slower recovery. Also considered should be the "goals and preferences of individual patients."
After a heart attack, infusing stem cells into the coronary arteries that supply blood to the heart muscle leads to a reduction in the area of heart damage. Moreover, heart function improves after the treatment, German physicians report.
Stem cells are early-stage cells that can go on to become several different types of tissue. Stem cells from the bone marrow or blood of 28 heart attack patients and about four days later infused the cells into the coronary artery that caused the heart attack.
The size of the damaged area of the heart fell significantly over the following four months. The reduction in damage size related directly to improvements in cardiac function.
Prior to the infusions, the investigators had assessed the capacity of the stem cells to migrate in response to chemical signals produced by the body. They found that migratory capacity, but not the number, of infused cells strongly predicted the reduction in size of the area of heart damage.
Therefore, "it might be useful to evaluate migratory capacity in order to predict functional improvement after infusion of the cells into patients hearts.
Risk factors for heart disease, such as high cholesterol and age, have a negative effect on the migratory capacity of the circulating stem cells, but lipid-lowering statin drugs can improve cell function, they added. Therefore, "current studies are focusing to determine the molecular mechanisms regulating the migratory capacity in order to optimize stem cell function."
In addition, they have a large ongoing program to treat patients with chronic heart failure in a similar way.
Researchers pointed out that large randomized trials are required to unequivocally demonstrate long lasting effects of this treatment.
Greater intake of magnesium -- one of the minerals recommended in a healthy diet -- appears to reduce the risk of heart disease, a study of more than 7,000 men shows.
Researchers note that although magnesium deficiency is believed to be detrimental for the heart, the association "has not been clearly identified."
In order to do so, the researchers examined dietary magnesium intake in 7172 men. At enrollment, the average daily dietary magnesium intake was 268 milligrams, with a range of 50 to 1138 mg.
During 30 years of follow-up, 1431 cases of coronary heart disease were identified.
Within 15 years of the first dietary assessment, the rate of heart disease was significantly lower in those with the highest daily magnesium intake (340 mg or more) compared with those with the lowest intake (186 mg or less).
The researchers calculate that the rate of heart disease was the equivalent of 4 cases per 1000 people per year for those in the high magnesium group, versus 7 cases among those with the lowest intake.
Further work needs to be undertaken to explore the value of magnesium supplementation. Our findings, however, are consistent with current guidelines for the intake of magnesium--along with the usual recommendations for exercise and a healthy diet. There is no magic bullet here."
Whether increases in dietary magnesium intake can actually alter the future risk of disease, warrants further study.



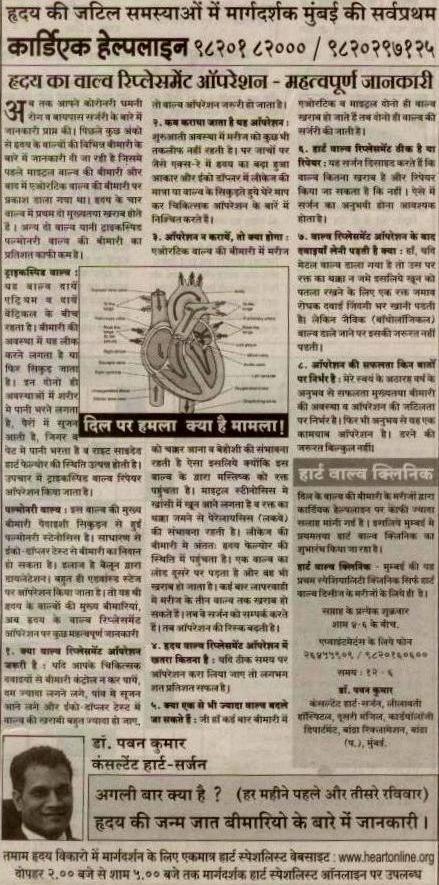
Heart Valve Disease & surgery - Gujarati article in Mid-Day